Preventing Complications in Hospital
The prevention of hospital acquired complications across East Metropolitan Health Service is an integral part of safety and quality improvement.
Throughout this section we provide information relating to hospital acquired complications (complications that people acquire while being cared for in our healthcare facilities) and how we can work together to reduce your chances of developing a complication while in hospital.
Our aim is always to provide people suffering from a medical condition with best-practice care and treatment while in hospital. However, sometimes in spite of the best care, other health or medical problems arise - either related to the primary diagnosis or related to care or treatment. This is referred to as a complication. A hospital-acquired complication (HAC) is a complication for which clinical risk mitigation strategies may reduce, but not necessarily eliminate, the likelihood of that complication occurring.
The national list of 16 HAC Groups was developed by the Australian Commission on Safety and Quality in Health Care through a comprehensive process that included reviews of the literature, clinical engagement and testing of the concept with public and private hospitals. The HACs list identifies agreed types of high-priority complications that clinicians, managers and others can work together to address and improve patient care.
The 16 HAC groups are:
- Pressure Injury
- Falls resulting in fracture or other intracranial injury
- Healthcare associated infection
- Surgical complications requiring unplanned return to theatre
- Unplanned intensive care unit admission
- Respiratory complications
- Venous thromboembolism
- Renal failure
- Gastrointestinal bleeding
- Medication complications
- Delirium
- Persistent incontinence
- Malnutrition
- Cardiac complications
- Third and fourth degree perineal laceration during delivery
- Neonatal birth trauma
Measuring hospital-acquired complication rates
Primary and secondary diagnoses and complications are routinely recorded for every admission in administrative databases after discharge. Analysis of this “coded data” provides health services with information about the occurrence of complications.
If one or more complications from the HAC Groups occurs during an admission, then that admission is counted as “an admission with one or more HAC” or “HAC Episode”. Sometimes there may be more than one complication from the same HAC Group, or complications from two or more different HAC groups.
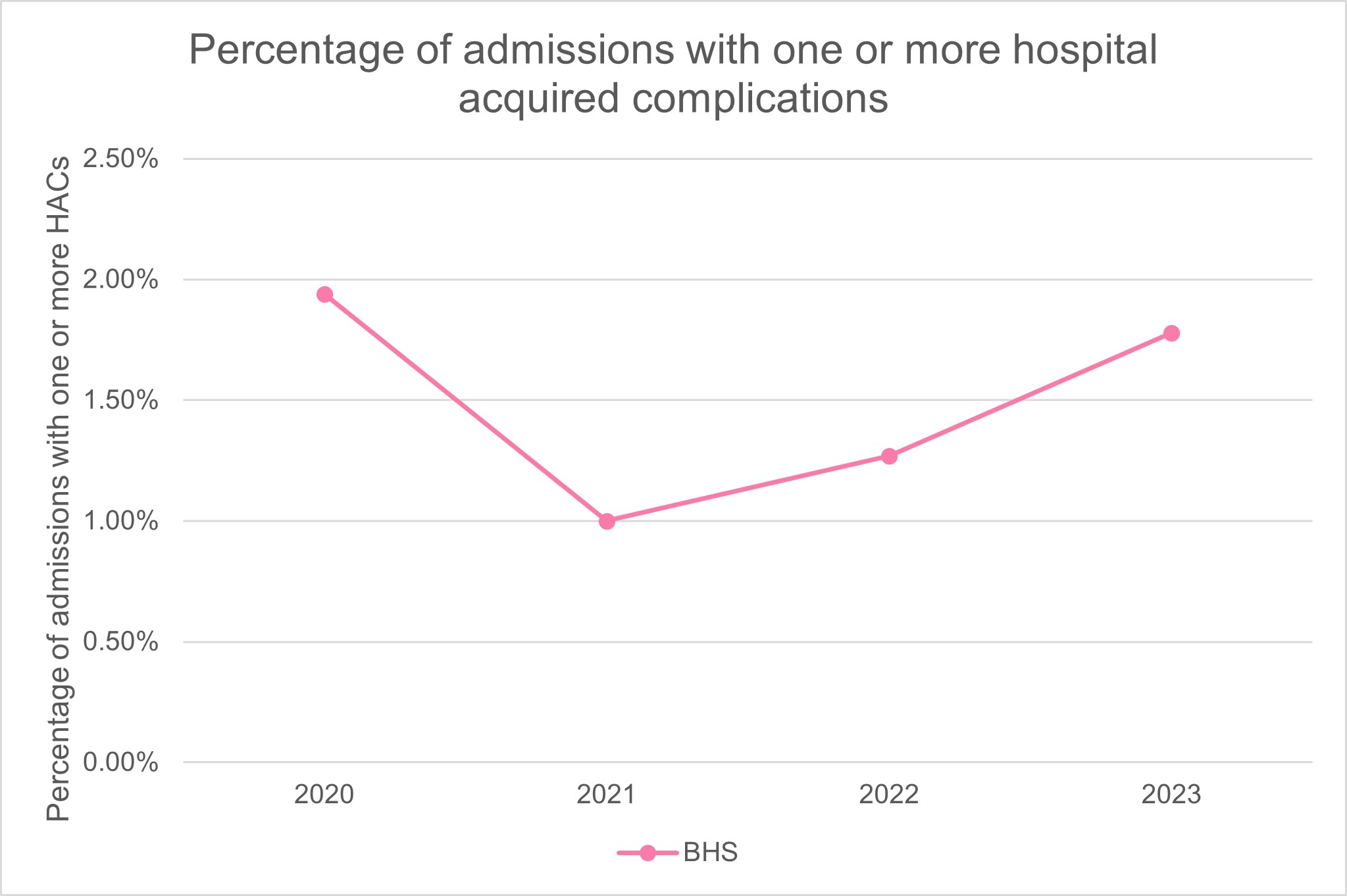
The chart that follows shows HAC Episodes (Groups 1-14 only) for Bentley Health Service combined as a percentage of all admissions per year since 2018.
How do we measure up
The graph below shows the percentage of admissions for Bentley Health Service.
Chart: Percentage of admissions with one or more hospital acquired complications.
What the figures mean
A lower percentage indicates fewer complications and is desirable. Although no benchmark has been set for this indicator, Bentley Hospital (BHS) constantly strives to reduce the number of hospital acquired complications through a broad range of improvement initiatives.
Each year nearly one quarter of people over 60 years of age will experience a fall. For some people, the injuries caused by their fall may be so serious that they can no longer live independently.
Falls account for over 80 per cent of all injury-related hospital admissions for people aged 65 years and older. They can occur at any age, but the frequency and severity of falls-related injuries increases significantly with age and frailty.
Unfortunately, falls are one of the most frequently reported clinical incidents in hospitals worldwide and it is known that there is a correlation with:
- length of hospital stay
- care and use of health resources
- discharge rates to a nursing home or residential care facility.
Measuring hospital-acquired complications – Falls
The World Health Organization (WHO) defines a fall as an event which results in a person coming to rest accidentally on the ground, floor or other lower level. This definition covers all types of falls-related clinical incidents, including:
- near-misses
- intercepted falls where the patient is lowered to the ground
- suspected/unwitnessed slips/trips/falls
- witnessed slips/trips/falls.
Fall-related injury is one of the leading causes of hospital-acquired morbidity and mortality in older Australians, and typically leads to pain, bruising and lacerations and fractures. Falls can also lead to intracranial bleeding, which can cause confusion, drowsiness, clouding, loss of consciousness and headache.
Healthcare commonly uses rates to measure complications such as these. The number of patients who have a fall in hospital resulting in fracture or intracranial injury per 1,000 patient days.
How do we measure up
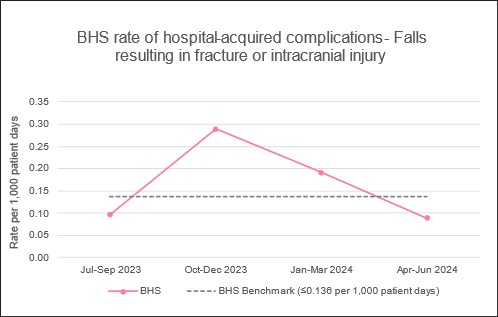
The graph below shows the combined rate of reported falls incidents for Bentley Health Service.
Chart: Rate of falls in hospital resulting in fracture or intracranial injury.
What the figures mean
The benchmark is less than or equal to 0.136 falls in hospital resulting in fracture or intracranial injury per 1,000 patient days. A rate lower than the benchmark is desirable.
BHS rates were below the benchmark for two quarters out of the last four quarters. BHS constantly strives to reduce the rate of falls incidents and preventative strategies continue to be put in place.
A pressure injury is a sore, break or blister of the skin caused by unrelieved pressure or friction on an area of the body over a period of time. The depth of skin damage can vary from shallow to very deep. Pressure injuries can be very painful and take a long time to heal. They may also reduce a patient’s mobility.
Older people are at most risk of pressure injuries, but they can occur in any patient or in any setting, including:
- acute areas such as operating theatres
- during transportation to a hospital
- intensive care units.
The majority of pressure injuries are preventable; however those at greater risk include the frail, elderly or people who have:
- been confined to a bed or chair
- poor bladder or bowel control
- diabetes, poor circulation or a history of smoking
- reduced mental awareness due to illness, medications or anaesthetics
- poor diet or fluid intake.
Pressure injuries may impact significantly on a patient’s:
- length of hospital stay
- comfort and quality of life
- cost of care and health outcomes.
Measuring hospital-acquired complications – Pressure injury
The international pressure injury classification systems provide a consistent and accurate means to communicate and document the severity of a pressure injury between clinical staff. The classification system grades these types of wounds in stages depending on:
- changes in the patient’s skin
- the depth of the injury
- whether there is any fluid draining from the wound.
Healthcare commonly uses rates to measure complications such as these. The number of patients who developed one or more Stage 3 or greater pressure injuries during their hospital stay per 1,000 patient days.
How do we measure up
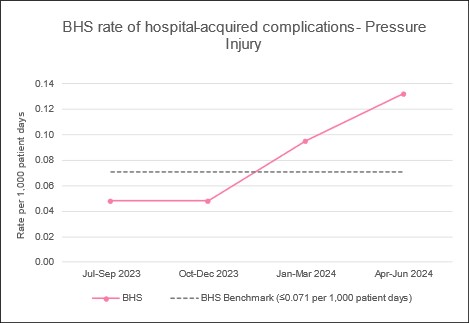
The graph below shows the combined inpatient pressure injury rate for Bentley Health Service.
Chart: Rate of hospital-acquired pressure injuries.
What the figures mean
The benchmark is less than or equal to 0.071 hospital-acquired pressure injury per 1,000 patient days. A rate lower than the benchmark is desirable.
BHS rates were below the benchmark in two quarters out of the last four quarters. BHS constantly strives to reduce the rate of hospital-acquired pressure injury and preventative strategies continue to be put in place.
Medicines are the most common treatment used in health care and contribute to significant improvements in health when used appropriately. However, because they are the used in complex healthcare environments – and despite the policies and procedure in place – there has been times when an error or adverse event has occurred.
Medication complications may indicate a failure in the medication management process that leads to, or has the potential to lead to, harm to the patient. Hospital-acquired medication complications prolong the length of hospitalisation, which impacts on patients and their families.
Medication complications can occur when:
- choosing a medicine
- writing the prescription
- preparing or manufacturing the medication
- dispensing the medication
- administering or taking the medication
- monitoring post-administration of the medication to the patient.
Measuring Hospital-acquired complications – Medication complications
Healthcare commonly uses rates to measure complications such as these. The number of patients who had a hospital-acquired medication complication during their hospital stay per 1,000 patient days.
How do we measure up
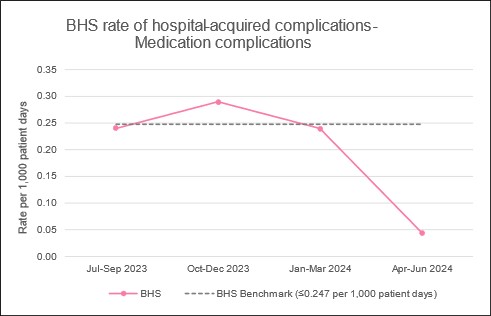
The graph below shows the combined medication related incidents rate for Bentley Health Service.
Chart: Rate of hospital-acquired medication complications.
What the figures mean
The benchmark is less than or equal to 0.247 hospital-acquired medication complications per 1,000 patient days. A rate lower than the benchmark is desirable.
BHS rates were below the benchmark in three quarters out of the last four quarters. BHS constantly strives to reduce the rate of hospital-acquired medication complications and preventative strategies continue to be put in place.

